字幕與單字
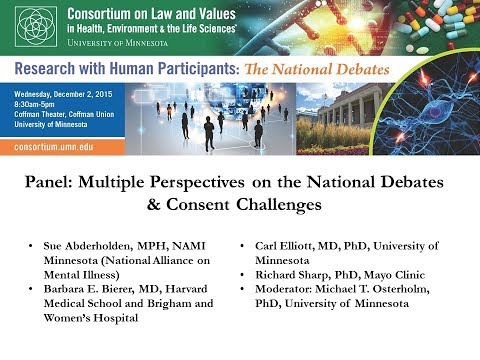
小組討論。關於國家辯論的觀點,研究倫理中的同意挑戰 (Panel: Perspectives on National Debates, Consent Challenges in Research Ethics)
00
林宜悉 發佈於 2021 年 01 月 14 日收藏
影片單字
vulnerable
US /ˈvʌlnərəbəl/
・
UK /ˈvʌlnərəbl/
- adj.脆弱的;易受攻擊的;易受傷的;脆弱的;易受影響的;需要特別照顧的;易受批評的;(橋牌中)易受攻的
B1 中級高級英檢
更多 使用能量
解鎖所有單字
解鎖發音、解釋及篩選功能
