字幕與單字
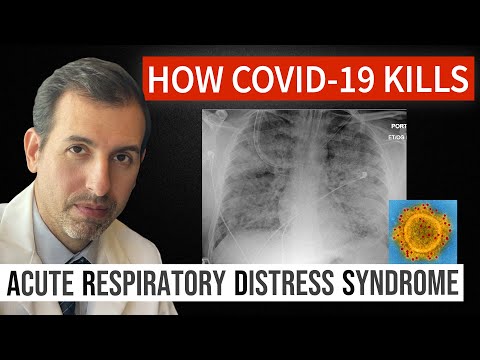
冠狀病毒是如何殺死。急性呼吸窘迫綜合症(ARDS)及治療方法 (How Coronavirus Kills: Acute Respiratory Distress Syndrome (ARDS) & Treatment)
00
Mia Chang 發佈於 2021 年 01 月 14 日收藏
影片單字
respiratory
US /ˈrɛspərəˌtɔri, -ˌtori, rɪˈspaɪrə-/
・
UK /ˈrespərəˌtɔ:ri:, -ˌtəʊri:, rɪˈspaɪərə-/
- adj.呼吸的;呼吸作用的
- n.呼吸醫學;呼吸系統;呼吸功能;呼吸窘迫;呼吸道疾病
C1 高級
更多 使用能量
解鎖所有單字
解鎖發音、解釋及篩選功能
